Radiation Therapy Quality Assurance: Why to Automate?
In radiation therapy (RT), where precision and efficiency can mean the difference between life and death, test automation is no longer a luxury—it has become a necessity. By overcoming the limitations of manual quality assurance (QA), automation delivers faster, repeatable, more accurate, and scalable processes that enhance patient safety and treatment quality and can increase patient throughput without compromising efficacy.
With evolving RT technologies in particle accelerators, imaging systems, sophisticated planning software and others, the complexity of quality assurance has increased.

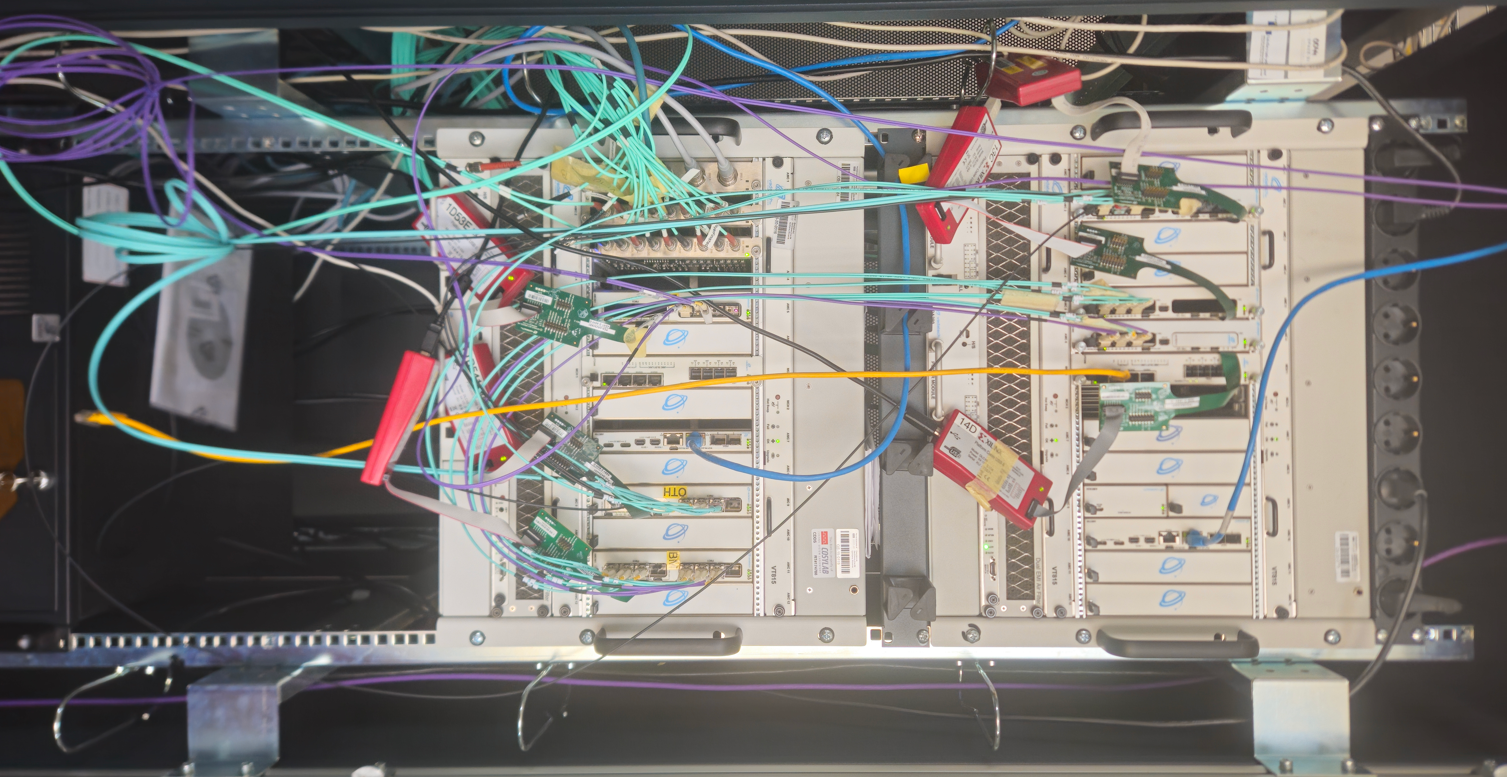
Closeup of Cosylab’s testing system for a dose delivery system (DDS).
Key Challenges in Manual QA Processes in Using Radiation Therapy Equipment
Manual quality assurance (QA) has been the foundation of radiotherapy safety and reliability for decades. However, today’s growing patient loads and increasingly complex technologies are exposing the limitations of these traditional processes.
- Time-Intensive Workflows
Manual QA involves multiple, detailed steps such as equipment calibration and treatment plan checks that can take hours per patient. This slows clinical workflows, reduces daily treatment capacity, and delays patient access. - Risk of Human Error
Even experienced professionals can make mistakes. The complex and repetitive nature of manual QA makes it easier to miss things, which can throw off treatment accuracy and put patients at risk. - Inconsistency and Variability
Results often vary depending on who performs the QA, leading to inconsistencies in process and quality. Standardising outcomes is difficult when operator experience, attention, and interpretation differ. - Limited Scalability
Manual processes don’t scale well with rising demand. As clinics see more patients and adopt advanced treatment techniques, the burden on QA teams grows—often without a matching increase in resources. - Systemic Barriers
Cancer remains a significant public health challenge and a national health priority in many countries worldwide. Politicians talk and promise, but the reality is that many healthcare systems still face shortages in radiotherapy machines, trained personnel, and long-term investment. These gaps make it even harder to sustain quality care using resource-heavy manual QA approaches.
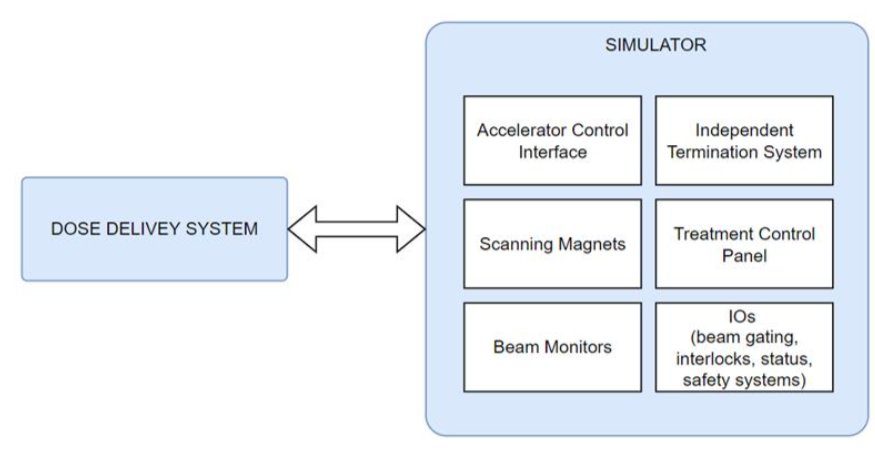
Schematic of the DDS-Simulator testing rig.
A Cosylab Use Case of Automated QA
The test system, presented in this blog’s images, simulates key subsystems of a radiotherapy Dose Delivery System (DDS) for an ion therapy device, allowing for comprehensive verification without real hardware.
It includes simulated interfaces for Accelerator Control, Scanning Magnets, Beam Monitors, IOs (including beam gating, interlocks, and safety systems), an Independent Termination System, and a Treatment Control Panel.
The setup enables automated and repeatable QA, making it ideal for development, validation, and training use cases.
How does Test Automation aid the Radiotherapist?
Test automation uses software-driven systems to perform routine, daily scheduled QA tasks faster and more accurately.
It reduces manual effort and increases consistency and reliability. Automated systems reduce radiotherapist error and make it easier to collect, track, and analyse data, helping to improve quality and provide the reports needed for audits and regulations.
Over the past decade, automation in radiotherapy has shown clear benefits. For example, publish-subscribe systems trigger QA checks automatically after updates or changes, reducing manual work and speeding up critical tests.
Another example is software tools, which fetch data from multiple systems into one platform, simplifying analysis and freeing staff to focus more on patient care.
Feature Comparison: Manual vs. Automated QA
Automated radiation therapy quality assurance is quite different from manual QA. Manual QA takes a long time because of its many steps, while automation speeds things up and gets treatments ready faster. Manual QA also tends to have more mistakes, while automated systems lower risks by being consistently accurate. Plus, manual results can change depending on who’s doing it, while automation keeps everything the same every time.
Scaling manual QA systems is also more time-consuming than increasing the size of automated solutions, which adapt smoother to growing demand.
Modern QA systems are automated and integrated. This makes them faster and more organised than traditional workflows and contributes to streamlining everything from planning to compliance, accelerating innovation and enhancing decision-making.
| Challenge | Manual QA | Automated QA |
| Time-Consuming Procedures | Hours-long delays in treatment | Minutes-long checks, faster treatment setup |
| Human Error | Risk of mistakes imperilling safety | Error reduction through precise automation |
| Inconsistent Results | Operator-dependent variability | Uniform, standardised outcomes |
| Scalability Issues | Limited by staff availability | Scales effortlessly with patient volume |
Table 1: Challenges and Solutions Through Automation
Cosylab’s Example:
Digital Twin & Simulation Technologies in QA
One of the ways we are implementing the concept of digital twins and simulation technologies “at home” in Cosylab is by using it in our testing and development processes. This helps us reduce development cycles by simulating medical device performance in software before progressing to physical prototyping.
Cosylab uses digital twins—virtual versions of real devices—to test and tweak products before they’re even built. This cuts down on time and costs while making things more reliable. Engineers replicate devices and their communication using simulation tech, catching problems early and improving customer support with tools like predictive maintenance and remote fixes.
The digital twin mirrors how a radiotherapy machine works in real-time, letting engineers test different scenarios without expensive physical models. To make this happen, Cosylab relies on FPGAs and PLCs. FPGAs act as fast simulators, copying device behaviour for real-time insights—perfect for testing sensors or processors. PLCs, common in automation, mimic industrial machinery logic, helping engineers check performance and avoid risks before launch.
This method spots issues early, saves resources, and meets demanding medical and industry standards. By bringing FPGA and PLC-based simulations into the mix, Cosylab has turned the slow, traditional design into a quick, cost-effective process that gets products to market faster. It’s a practical, hands-on way to build better software for radiation therapy devices.
Based on our experience with automated test procedures, we develop customised QA systems that verify the correct functioning of all critical treatment subsystems of a radiotherapy machine—including the main control system—before patient treatments begin each day. This includes automated testing using actual or simulated subsystems such as the couch, gantry, beam monitoring devices, and linac, ensuring the system performs safely and accurately in clinical conditions.
(Leo Cancer Care, Crawley, UK and HFCIM, Hefei, China).
Future Trends and Conclusion
Automated QA in radiotherapy increases productivity for radiation oncology wards since these advancements also align QA with innovations (like adaptive and flash radiotherapy), driving quality and safety.
Here are some key trends to watch.
- AI-Driven Quality Assurance: Artificial intelligence (AI) and machine learning (ML) are increasingly being used to predict anomalies in treatment plans and delivery systems before they occur. This proactive AI approach of informing QA procedures of its insights enhances patient safety and treatment accuracy, helping medical physicists improve innovative treatments and speed up conventional ones.
- Real-Time Monitoring: Radiation oncology staff using automated systems can continuously oversee treatment and detect and correct deviations instantly. With this, treatment delivery will be more efficient, precise and repeatable, with fewer errors.
- Scalability and Flexibility: As patient numbers climb, automation can support oncologists in diversifying treatment protocols, increasing throughput without strain, streamlining operations, and easing hospital administration. Automated QA adds the ability to handle many QA scenarios — many more than in manual testing – which are tailored to the treatment needs.
- Integration with Emerging Therapies and Modalities: Acquiring and integrating innovations such as adaptive and flash radiation therapy and personalised dosing will become smoother with automation because the QA system will already be in sync with clinical advancements.
 Test environment for the DDS of an ion therapy device; left simulator, right DDS.
Test environment for the DDS of an ion therapy device; left simulator, right DDS.
Conclusion
Today, precision and efficiency are of utmost importance in radiotherapy.
Automating radiation therapy quality assurance is one of the transformative technologies that help clinics accelerate therapy delivery, maintain regulatory compliance, and increase consistency.
This means safer, quicker, and more effective therapies for patients while offering clinicians a seamless and scalable workflow.
Test automation isn't just a patch of an existing process—it's a cornerstone of radiotherapy's more effectual and affordable future.
About the author
Primož Napotnik leads a team focused on development and test automation for PLC and FPGA platforms in safety-critical systems. The team automates to a level that frees them up for high-impact work—and occasionally for well-earned fun time.